What Health Care Providers Should Know about Patients’ Hesitancy to Seek in-Person Care
As we mark the one-year anniversary since the U.S. federal government declared the COVID-19 outbreak a national emergency, there is greater understanding of the virus, improved protection measures, and the rollout of vaccines. At the same time, COVID-19 cases and related deaths continue in the U.S. In another worrisome trend, Americans continue to delay preventive medical care during the pandemic. By getting recommended preventive care—for example, immunizations and screenings for cancer and high blood pressure—individuals can reduce their risk for diseases, disabilities, and death. Without preventive care, individuals are at greater risk for diseases and decreased life expectancy.
Recent findings from the U.S. Census Bureau’s Household Pulse Survey found that nearly one-third of Americans delayed seeking health care in the last four weeks because of the pandemic. Meanwhile, the Health Care Cost Institute notes that as of Dec. 1, 2020, the rate of childhood immunizations was approximately 6 percent below 2019 levels and colonoscopies are 12 percent below pre-pandemic levels. According to a Commonwealth Fund analysis, visits to dermatologists and adult primary care providers have increased and even exceeded pre-pandemic levels, but visits to many clinical specialists, such as pulmonologists, otolaryngologists, and behavioral health providers, have decreased by more than 10 percent.
- Conducted between Oct. 1 and Oct. 20, 2020
- 1,016 adults age 18 and older residing in the U.S.
- Used the Ipsos KnowledgePanel®
In fall 2020, the American Institutes for Research conducted a nationally representative survey to better understand how people living in the U.S. feel about receiving in-person health care during the pandemic. According to the survey, just over one-third of Americans said that the risk of contracting COVID-19 makes them less likely to go to a health care provider or dentist for check-ups or wellness care. Those survey findings showed the reluctance to receive in-person care was more pronounced among Hispanic respondents (53 percent) and those who reported they were at high risk for developing a severe sickness if exposed to COVID-19 (45 percent).
What Would Make Patients More Comfortable Receiving Preventive Care in Person?
Considering the decline in preventive care services and the continuing pandemic, it is important that health care providers ensure that their patients understand the continued need for preventive care and the efforts health care providers and systems have taken to make health care seeking behavior safe. Because they have likely established trust with their patients, providers are best positioned to communicate when a patient should receive in-person care or whether telehealth is sufficient. AIR’s survey provides further insight into steps providers can take to ease patients’ discomfort with in-person care. Here’s what providers should know.
Respondents reported several worries about aspects of in-person health care settings. More than half (56 percent) of respondents reported they were concerned about other patients not wearing masks, approximately 40 percent were concerned with having physical contact with or proximity to other patients, and 35 percent expressed concern about the cleanliness of the health care facility. Across each of these aspects, non-white respondents were consistently more likely than white respondents to report being extremely concerned.
Respondents reported they would feel safe seeking in-person medical or dental care if health care providers and others took certain actions in health care settings. AIR asked respondents to identify the top three actions providers could take, and what they reported was similar with their concerns about other patients not wearing masks and facility cleanliness.
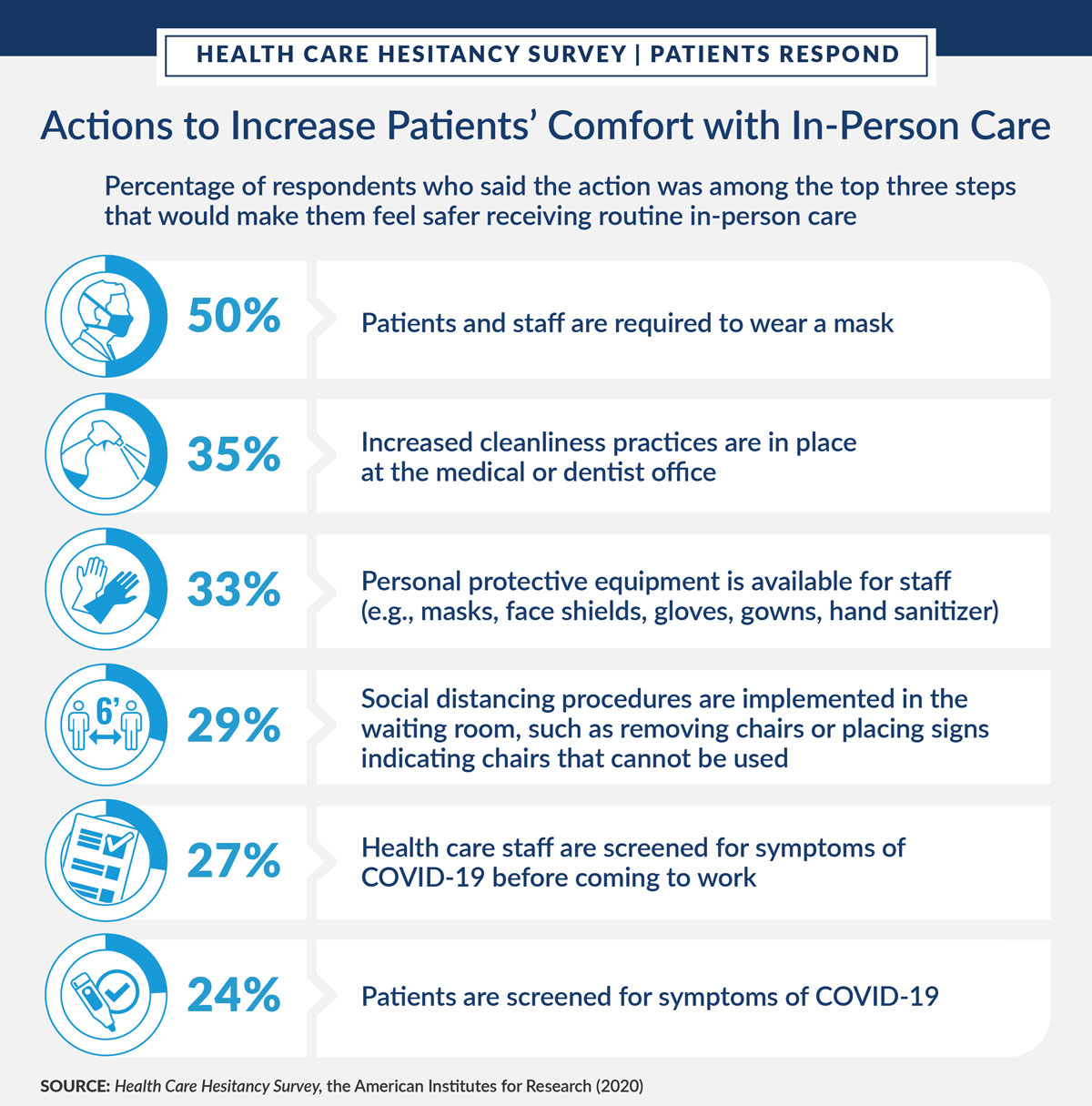
AIR’s survey findings provide health care systems and providers with insight into which policies they should emphasize when they communicate about routine and preventive care with patients—in particular, racial minorities and individuals with chronic conditions that put them at higher risk for complications from COVID-19. These findings show that providers should emphasize their mask-wearing policies and discuss their approaches to cleanliness and social distancing, as well as staff’s use of personal protective equipment. Health care systems and providers should conduct broad outreach to their patients and communities to encourage them to seek routine, preventive care as the COVID-19 pandemic continues. The Centers for Medicare & Medicaid Services and professional organizations such as the American Medical Association have developed guidance that health care systems and providers can use to help alleviate patient concerns as they communicate with patients about scheduling preventive care.
Communicating with patients about the COVID-19 safety practices in medical and dental offices is a way for providers to increase patient trust and confidence in seeking routine and preventive care during the pandemic. It is also key that providers educate patients about the importance of being up to date with preventive and routine care. This level of patient-provider communication and transparency may help address patient concerns about in-person care safety and contribute to improving preventive care overall.
The next piece in this series will cover how policymakers and providers can collaborate to address the preventive care topic of vaccine acceptance.
