How Willing Are People in the U.S. to Seek Health Care During the COVID-19 Pandemic?
The importance of continuing to seek health care services during the ongoing pandemic is underscored by a growing body of evidence that there has been an increase in excess deaths (the difference between the expected and actual number of deaths). One study found that between March 1 and Aug. 1, 2020, the U.S. experienced a mortality rate 20 percent higher than expected, with increases in deaths attributable to non-infectious conditions, such as Alzheimer’s disease, dementia, and heart disease.
Besides the direct impact of COVID-19 on daily life, the pandemic has affected how individuals approach their personal health and well-being, including if and how they seek health care services.
Many health care services must take place in person. For example, routine dental care takes place in person, as do cancer screenings and disease management (e.g., infusions and dialysis). Patients also must visit a provider’s office or a clinical laboratory in person for diagnostic tests or to have blood drawn to monitor chronic illnesses. In addition, childhood, influenza, pneumococcal, and other immunizations must be administered in person.
According to a recent study, office visits to primary care providers and specialists declined by almost 60 percent in the first few months of the pandemic. As of October 2020, primary care and specialist visits generally returned to pre-pandemic levels; however, office visits for younger children remain low, as do visits to some specialists (e.g., pulmonologists, otolaryngologists, and cardiologists).
How Willing are People in the U.S. to Seek In-Person Care?
To better understand how people living in the U.S. feel about receiving in-person health care during the pandemic, the American Institutes for Research conducted a nationally representative survey between Oct. 1 and Oct. 20 of 1,016 adults age 18 and older residing in the U.S., using the Ipsos KnowledgePanel®. The findings from this survey provide valuable insights to inform providers and policymakers about what prevents individuals from seeking care. Using these findings, providers and policymakers will be able to address the factors that inhibit individuals from seeking necessary in-person care to encourage more people to receive needed health services during this time. Our initial analysis reveals differences among respondents in their concern about receiving in-person health care services.
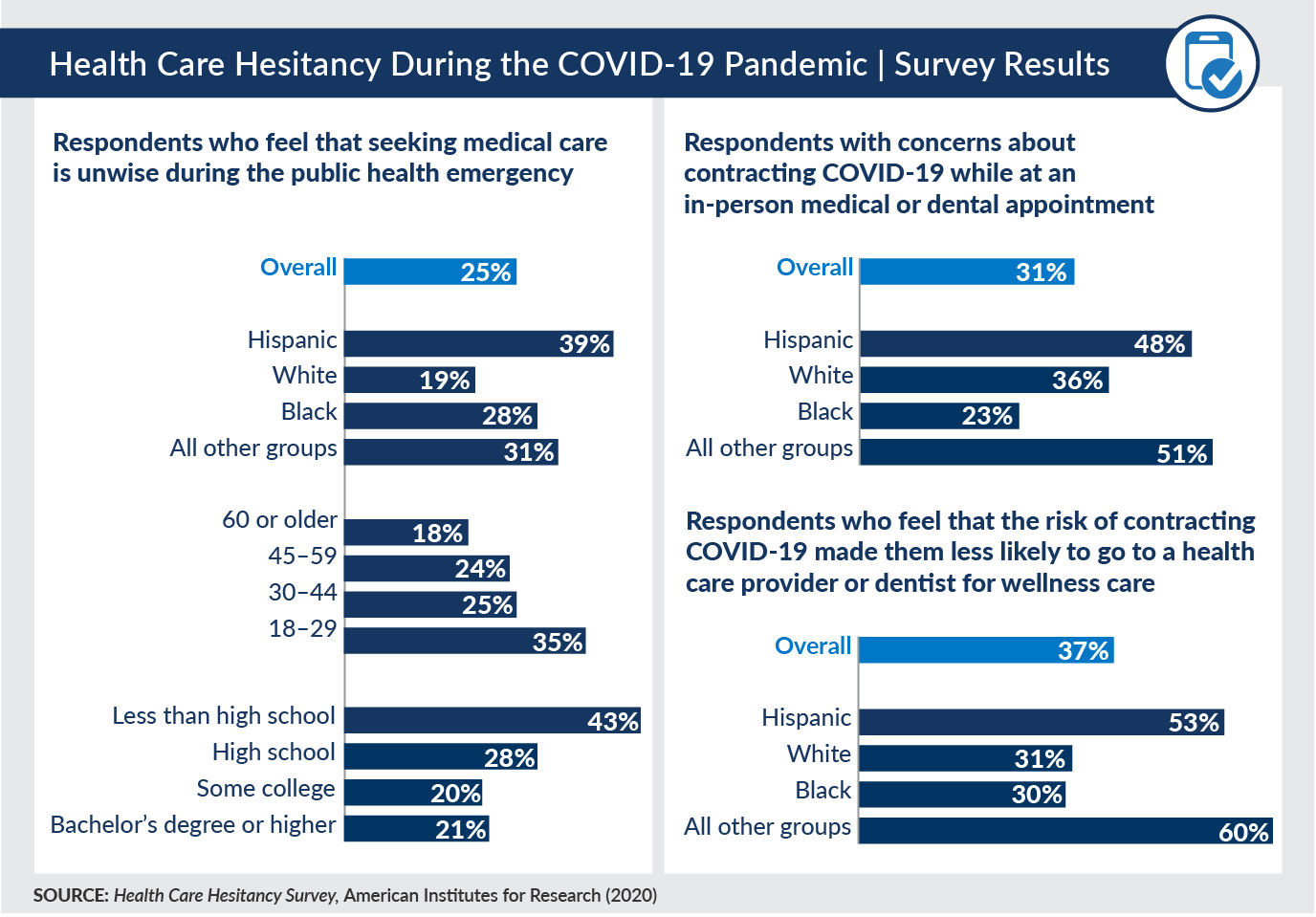
A little more than one-third (37 percent) of all respondents agreed that the risk of contracting COVID-19 made them less likely to go to a health care provider or dentist for wellness care. A larger percentage of Hispanic, Black, and other non-white respondents (compared with white respondents) agreed that they were less likely to go to a provider for wellness care during the pandemic.
We also asked respondents to rate how concerned they were that they would contract COVID-19 while at an in-person medical or dental appointment. Overall, 31 percent of respondents expressed some level of concern. Persons of color had higher rates of concern compared to white respondents.
Our survey also found that one in four (25 percent) respondents agreed with the statement, “It is unwise to seek medical care right now. Healthcare providers need to treat those infected with COVID-19.” Younger respondents, respondents with lower levels of education, and Hispanic respondents were the most likely to agree with this statement.
Implications of Continued Reluctance to Seek In-Person Health Care Services
Preliminary findings from our survey demonstrate a need to address care-seeking behavior during the pandemic and provide evidence-based information about the safety of in-person care and the precautions providers are taking. The potential negative impact of avoidance of care—particularly among Black, Hispanic, and other non-white populations—could have long-term effects. Persons of color are less likely to have access to preventive care, resulting in an increased likelihood of having chronic conditions.
U.S. residents will benefit from receiving evidence-based informational material that highlights the advantages and importance of continuing to seek routine health care during the pandemic. These materials should be tailored to the needs of individual groups, especially people of color, those with less than a high school education, and younger adults.
Longstanding racial and ethnic health disparities, coupled with higher rates of COVID-19 infections in under-resourced communities, could put additional strains on the health care system. Some communities may experience increased rates of chronic condition complications because of patients delaying or foregoing care during the pandemic. Many primary care providers across the country are already stretched thin from responding to COVID-19 and will have to overcome logistical challenges when redesigning how they deliver care in the wake of the pandemic, in particular how they educate and deliver care to patients with chronic conditions.
